Welcome to Crohn’s and Colitis Awareness Week, a time dedicated to shedding light on two significant and often misunderstood conditions. But what exactly are these diseases? Crohn’s disease is a chronic inflammatory bowel disease (IBD) that primarily affects the digestive tract, presenting challenges that go beyond typical digestive issues. Colitis refers to the chronic inflammation of the inner lining of the colon, another form of IBD with its own unique set of difficulties.
The shared characteristics of these chronic diseases not only place them under the umbrella of IBD and autoimmune disorders but also result in similar, often debilitating symptoms that impact patients both physically and emotionally. However, comprehending these diseases extends beyond mere symptom recognition. It involves an understanding of personal risk factors, essential for early detection and potentially altering the disease’s progression significantly. By recognizing that awareness is a transformative force, you can reduce the impact these conditions have on your life.
Navigating the Nuances: Comparing Crohn’s Disease and Ulcerative Colitis
Crohn’s disease is characterized by inflammation of the gastrointestinal tract. It can affect any part of the tract from mouth to anus, but it most commonly targets the end of the small intestine and the beginning of the colon. Although there is no cure for Crohn’s disease, various treatments exist to reduce symptoms and improve the quality of life for those affected. Ulcerative colitis, the type this article will be focused on, is the most common form of colitis. Characterized by recurring inflammation of the colon and rectum, ulcerative colitis shares similarities with Crohn’s, including the absence of a cure. Yet, like Crohn’s, it can be managed with treatments designed to control symptoms and sustain remission.
What Causes Crohn’s and Colitis?
The precise cause of Crohn’s disease remains elusive, though genetic predisposition, environmental influences, and immune system factors are known contributors. Having a family history of Crohn’s increases your risk of developing the disease. Another significant factor in Crohn’s disease is the body’s immune system, which, rather than solely defending against pathogens, mistakenly attacks the cells of the gastrointestinal tract. This atypical immune response may be influenced by a range of factors, such as dietary habits, smoking, and urban living conditions, including pollution, elevated stress levels, and economic pressures. Additionally, changes in the gut microbiome–the complex community of bacteria within the digestive tract–are believed to play a crucial role in initiating this misguided immune activity.
The suspected causes of ulcerative colitis closely mirror those of Crohn’s disease, including the potential for an abnormal immune response. In this scenario, the immune system targets the lining of the colon, resulting in inflammation. Ulcerative colitis is also more common among those with a family history of the disease and is likewise triggered by diet, lifestyle, and pollution. Changes in the gut microbiome might also play a role in kick-starting the disease.
Decoding Crohn’s and Colitis Symptoms
Given the shared range of causes, it’s no surprise that Crohn’s and colitis symptoms are also quite similar. Both conditions cause abdominal pain, diarrhea, rectal bleeding, weight loss, anemia, and fatigue. However, a particularly notable (and unfortunate) symptom unique to ulcerative colitis is a heightened urgency to defecate.
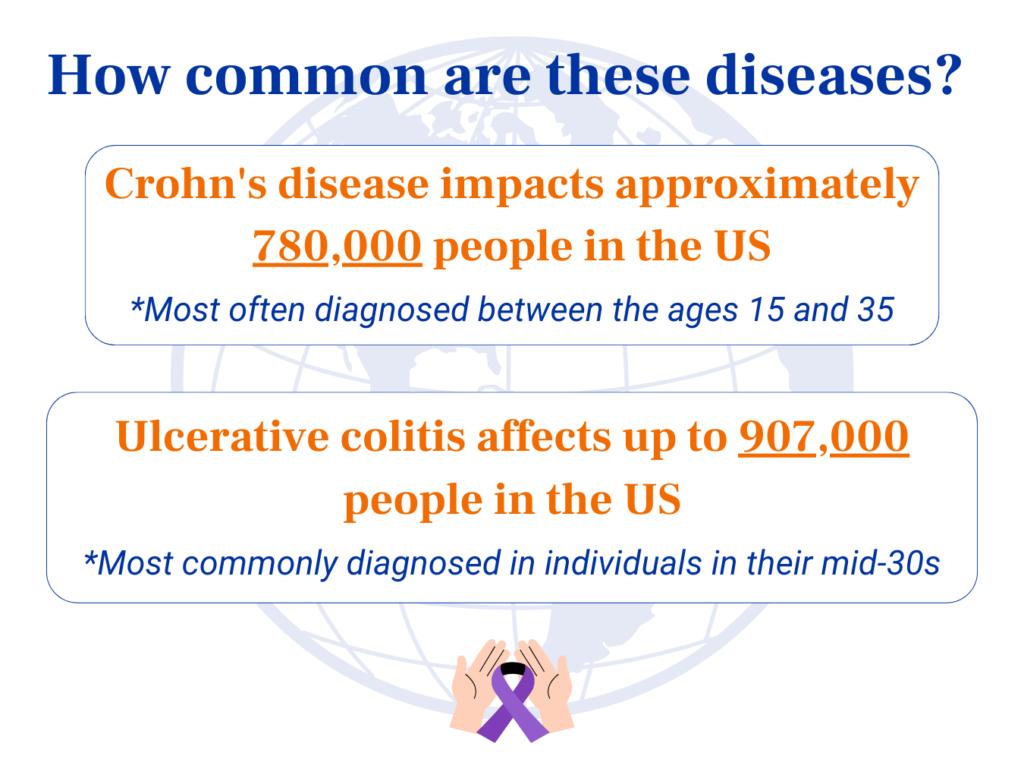
Crohn’s disease affects up to 780,000 people in the United States. It can come about at any age but is typically diagnosed in teens and young adults between the ages of 15 and 35. On the other hand, ulcerative colitis impacts up to 907,000 individuals in the U.S. While its prevalence mirrors Crohn’s disease in terms of geographic and demographic patterns, it is most commonly diagnosed in individuals in their mid-30s, though it too can occur at any age.
It’s important to understand that while Crohn’s disease and ulcerative colitis share similarities, one does not lead to the other. However, due to the overlap in symptoms and the complexity of these conditions, a diagnosis may be reevaluated and changed over time. Sometimes, what’s first thought to be one type of IBD might actually be the other, showing just how tricky it can be to properly diagnose and understand these conditions.
Navigating Life with Crohn’s and Ulcerative Colitis
Living with Crohn’s and colitis is no doubt a challenging feat. The constant need for restroom access, a common requirement with both conditions, can be draining. These conditions often leave you too fatigued to socialize with friends or fulfill work obligations. Crohn’s and colitis can also take a toll on mental health, leading to anxiety, depression, stress, and even a sense of loneliness when it feels like others can’t understand your experience.
Though medications can help keep your symptoms at bay, side effects like infections, skin reactions, and mood and bone density changes can throw a wrench in your daily routine. Serious health issues can unfortunately come from these conditions, like blockages in your bowels and fistulas as well as a higher chance of colon cancer. Juggling doctor visits and medications can be daunting too, not to mention the hit your wallet takes from treatment costs and potentially losing time at work.
Managing Nutrition, Checkups, and Stress
Regular medical checkups are the cornerstone for effectively tracking your condition and treatment progress. This includes crucial screenings for serious complications like colon cancer.
Nutrition also plays a crucial role in symptom management. Eating smaller, more frequent meals and keeping a food diary can help manage symptoms, along with nutritional supplements when necessary. It’s essential to identify and steer clear of trigger foods such as the following:
- High-fiber foods
- Dairy products and gluten
- Fatty, greasy, spicy, or processed foods
- Alcohol, caffeine, and carbonated beverages
- Non-absorbable sugars
Stress management is key, using methods like meditation, yoga, and deep breathing, supplemented by therapy or support groups. Engaging in regular, moderate exercise boosts overall health and helps manage stress. Quitting smoking is especially vital for those with Crohn’s, as it can worsen the condition.
Medication can help you manage Crohn’s and ulcerative colitis, with options ranging from anti-inflammatory drugs like aminosalicylates and corticosteroids, to immune system suppressors, biologics for targeted therapy, antibiotics for secondary infections, and medications for symptom relief. In extreme cases, surgery may be required, like removing affected GI tract sections in Crohn’s or a total colectomy in ulcerative colitis to potentially cure the condition.
Resilience in the Face of Crohn’s and Colitis
As Crohn’s & Colitis Awareness Week wraps up, it’s important to recognize how much healthy lifestyle changes can transform the way we manage these conditions. Adopting a well-rounded approach that includes smart nutrition choices, routine checkups with your primary care, effective stress management, and medication when needed can greatly reduce the impact of Crohn’s and ulcerative colitis. Every step taken towards a deeper understanding and effective management of these conditions is a step forward in your health journey.
