In the complex world of our bodies, where each cell plays a critical role in maintaining homeostasis, the onset of lung cancer emerges as a jarring disruption. This disease takes root when mutations form in the DNA within our lung cells, multiplying uncontrollably and eventually forming a tumor. As the cancer cells grow, they move beyond their original location, affecting the healthy tissues around them. These cells can also break away and travel through the body’s blood and lymph system, leading to a dangerous spread called metastasis.
Lung cancer tops the chart for cancer-related fatalities worldwide. You’re likely aware that smoking is a primary culprit, but it’s far from the only one. Surprisingly, several under-the-radar risk factors might be quietly jeopardizing your health. In this post, we’ll unveil some of the lesser-known dangers associated with lung cancer. Read on not only to assess your own risk but also equip yourself with potentially life-saving knowledge.
Understanding the Fundamentals of Lung Cancer
The lungs play a crucial role in the human respiratory system. These two spongy structures ensure that oxygen is absorbed from the air we breathe and transferred into our bloodstream. Simultaneously, they help in expelling carbon dioxide from the blood, releasing it back into the atmosphere. Lung cancer can severely hinder the lungs’ ability to carry out these vital respiratory tasks.
There are two types of lung cancer. The first, Non-small cell lung cancer (NSCLC), is the more prevalent variety, accounting for approximately 85% of all cases. NSCLC encompasses several subtypes, including adenocarcinoma, squamous cell carcinoma, and large cell carcinoma.The second type, small cell lung cancer (SCLC) is less common but notably more aggressive. Constituting about 15% of all lung cancer cases, SCLC is notorious for its rapid progression, spreading more swiftly than its non-small cell counterpart.
You probably know that smoking is the leading cause of lung cancer, introducing a slew of harmful chemicals into the lungs with every puff of tobacco smoke. This not only damages lung tissue but can also create lasting genetic mutations. The journey from healthy to cancerous cells begins when these carcinogens assault lung cell DNA, hindering the body’s natural repair work. This interference can cause genetic errors, disrupting how DNA operates and replicates.
Smoking continuously irritates the lungs, leading to chronic inflammation and a surge in harmful oxidative stress and free radicals. These conditions set the stage for tumors to form and grow. The relentless nature of smoking gradually undermines lung cells, steering them from a healthy state toward a cancerous one. It also impairs the lungs’ self-cleaning features, particularly affecting the cilia, which are responsible for filtering out unwanted particles. This decline in lung defense amplifies the presence of carcinogens, heightening the chances of infections and cancer.
What You Don’t Know About Lung Cancer
Quitting smoking undeniably reduces your risk of developing lung cancer. But it does not completely erase the years of damage done by cigarettes. Long-term smoking causes a domino effect of DNA damage that can eventually lead to cancer—even after you’ve kicked the habit. That’s because carcinogens from tobacco smoke linger in the body, continuing to harm your cells. The defenses of the lungs, weakened by persistent smoking, may not fully bounce back even when you quit, maintaining a heightened vulnerability compared to those who have never smoked.
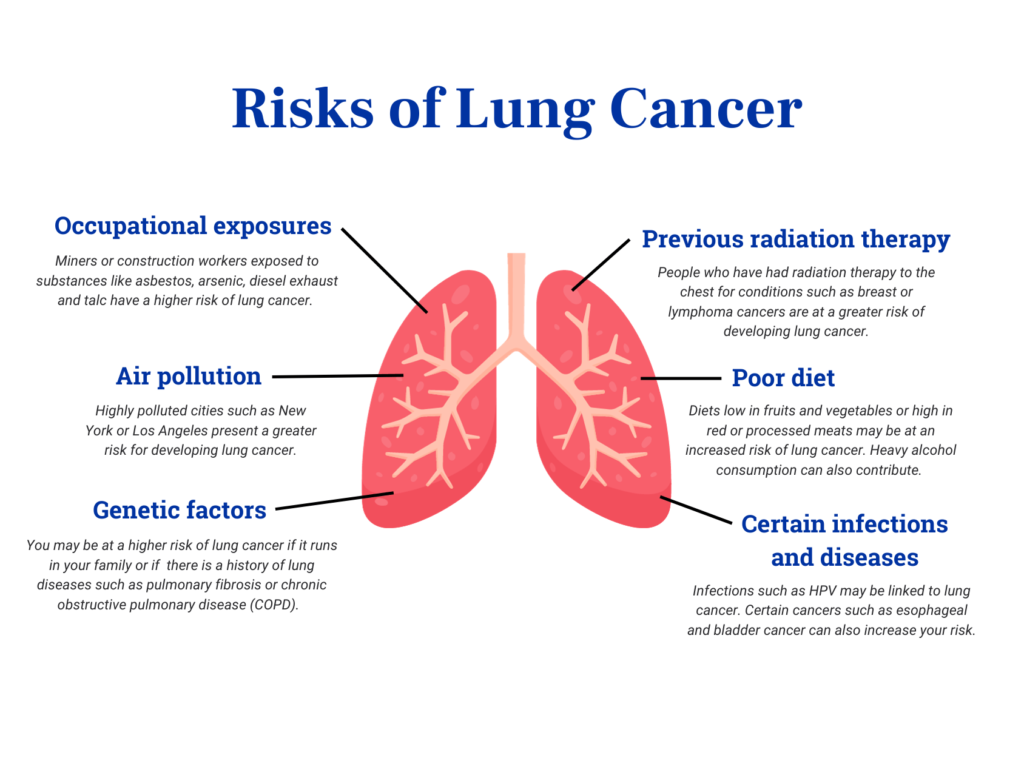
Another lesser-known cause of lung cancer is radon gas. This is an invisible and odorless radioactive substance that can seep into homes, schools, and offices through foundation cracks and even contaminate water from wells. As the second leading cause of lung cancer in the USA, radon’s radioactive byproducts can cling to the lung lining when inhaled. Secondhand smoke also poses a significant threat to non-smokers. In fact, those living with smokers or exposed to secondhand smoke in their workplace face a 20-30% higher risk of developing lung cancer.
The conversation around lung health often misses the risks associated with marijuana and vaping. Marijuana smoke, mirroring tobacco, is rife with carcinogens and tar, potentially causing DNA alterations in lung cells when inhaled deeply. While edibles and non-smokable forms are considered safer alternatives, vaping still raises concerns due to the inhalation of chemicals like formaldehyde, with the full implications of its long-term cancer risk yet to be determined.
Asbestos, a well-known industrial hazard, is a significant contributor to lung cancer because it can lead to tissue irritation, DNA mutations, and uncontrolled cell growth. Occupational lung cancer risks are particularly high in mining and manufacturing jobs due to frequent exposure to hazards like arsenic and diesel exhaust. City dwellers frequently exposed to air pollution also face increased risks.
A diet rich in red and processed meats and alcohol, or lacking in fruits and vegetables, correlates with a higher lung cancer risk. Supplements such as beta-carotene may further elevate this risk in smokers. Certain medical conditions and treatments, including infections like HPV, a history of esophageal or bladder cancer, or undergoing hormone replacement therapy could also contribute to a higher likelihood of developing lung cancer.
Navigating Lung Cancer with Hope
Lung cancer diagnosis often presents a stark reality, with only 26% of cases identified at an early stage. Most distressingly, 44% of lung cancer patients aren’t diagnosed until the advanced stages, facing a mere 7% survival rate. But amidst these daunting statistics, there glimmers a ray of hope. In the last five years, early lung cancer detection has increased by 17%, raising the survival rate from 21% to 25%. This encouraging trend underscores the importance of proactive measures to reduce lung cancer risk.
Here are some key strategies for defending yourself against lung cancer:
- Quit smoking and avoid secondhand smoke
- Test your home for radon
- Minimize exposure to toxic substances
- Avoid unnecessary X-rays
Maintaining a healthy diet rich in fruits, vegetables, and high levels of vitamins A and C may contribute to lowered risk. As can regular physical activity like aerobic exercises, strength training, yoga, and interval training. If you live in a heavily polluted area, reduce air pollution exposure by staying indoors on bad days, using air purifiers, and wearing masks. Recognizing early symptoms such as persistent cough, hemoptysis, shortness of breath, chest pain, and unexplained weight loss is also vital for early intervention. Additionally, keeping up with vaccinations is key in guarding against infections that might heighten the risk of conditions related to cancer.
Patients diagnosed with lung cancer have access to a wide array of treatment options, including surgeries such as lobectomy and radiosurgery, medical treatments such as chemotherapy and immunotherapy, and radiation techniques like EBRT and SBRT. Palliative care enhances life quality during treatment, while ablation provides a targeted way to kill cancer cells. These advancements, along with early detection and prevention, bring new hope to navigating lung cancer.
Taking Proactive Steps Against Lung Cancer
Catching lung cancer early and getting treatment fast is key to improving your chances of beating it. It’s also important to be aware of the lesser-known risks associated with certain jobs, environmental factors, and lifestyle choices. Steer clear of these risks when you can, and don’t skip your regular doctor visits and health screenings—they’re your best shot at catching problems early on. By staying on top of these things, you can really strengthen our fight against lung cancer and aim for a healthier life ahead.