Are you troubled by symptoms like heartburn, difficulty swallowing, or even vomiting? Do you often feel as if there’s a lump in your throat, or suffer from a persistent dry cough, hoarseness, or sore throat? Perhaps you’re frequently plagued by relentless burping or hiccups, a feeling of bloating, or nausea.
If these complaints sound familiar, you might be suffering from gastroesophageal reflux disease, or GERD. This condition is like having a faulty valve between your throat and stomach, allowing stomach acid to flow upwards. Let’s explore the causes of GERD, and provide insights into how you can effectively prevent and treat this discomforting condition.
Exploring the Major Factors That Lead to GERD
GERD is a digestive disorder characterized by the frequent backward flow of stomach acid into the esophagus, the tube that connects your throat to your stomach. This unwelcome backflow triggers not just discomfort but also persistent irritation and heartburn, often significantly impacting daily life. The main cause of GERD is a malfunctioning lower esophageal sphincter (LES), a muscular ring that separates the esophagus from the stomach.
The LES plays two key roles. First, it allows food and liquid to flow down into the stomach when you swallow. Second, it prevents the acidic contents of the stomach from flowing backward into the esophagus, which isn’t designed to handle constant exposure to stomach acid. If the LES is weak or relaxes inappropriately, it can lead to acid reflux or GERD.
Several factors can increase the risk of developing GERD:
- Hiatal Hernia: This is a condition where part of the stomach pushes through a larger-than-normal opening in the diaphragm, ascending into the chest cavity. Hiatal hernias not only disturb the usual link between the esophagus and stomach but also weaken the LES.
- Foods and Drinks: Consuming foods and drinks such as chocolate, peppermint, fatty foods, coffee, alcoholic beverages, and carbonated drinks can trigger GERD symptoms. Overindulging in these items may increase the likelihood of developing GERD.
- Medications: Some medications, including aspirin, certain antibiotics, and some antidepressants and sedatives, can cause acid reflux.
- Obesity: Excess weight puts additional pressure on the stomach, increasing the risk of developing GERD.
- Pregnancy: Hormonal changes during pregnancy can cause the muscles in the esophagus to relax more frequently. The increased pressure on the stomach can also contribute to GERD.
- Smoking: Smoking tobacco weakens the muscle that connects your throat to your stomach. This occurs due to substances in tobacco like nicotine and acetaldehyde, decreased saliva production, and damage to the stomach lining.
- Gastroparesis: This is a condition where the stomach takes longer than usual to empty its contents into the small intestine. Gastroparesis significantly raises the chances of stomach contents flowing back into the esophagus.
- Connective Tissue Disorders: Connective tissue disorders like Scleroderma, Ehlers-Danlos Syndrome, Marfan Syndrome, Lupus, and Rheumatoid Arthritis can lead to GERD.
Managing GERD with Better Health and Lifestyle Choices
Managing GERD involves adopting a healthier diet and daily habits, which are the primary methods for reducing your symptoms. If these approaches are not enough, exploring various medications and considering surgery might be the key to overcoming GERD’s challenges–let’s get into it.
Dietary Changes
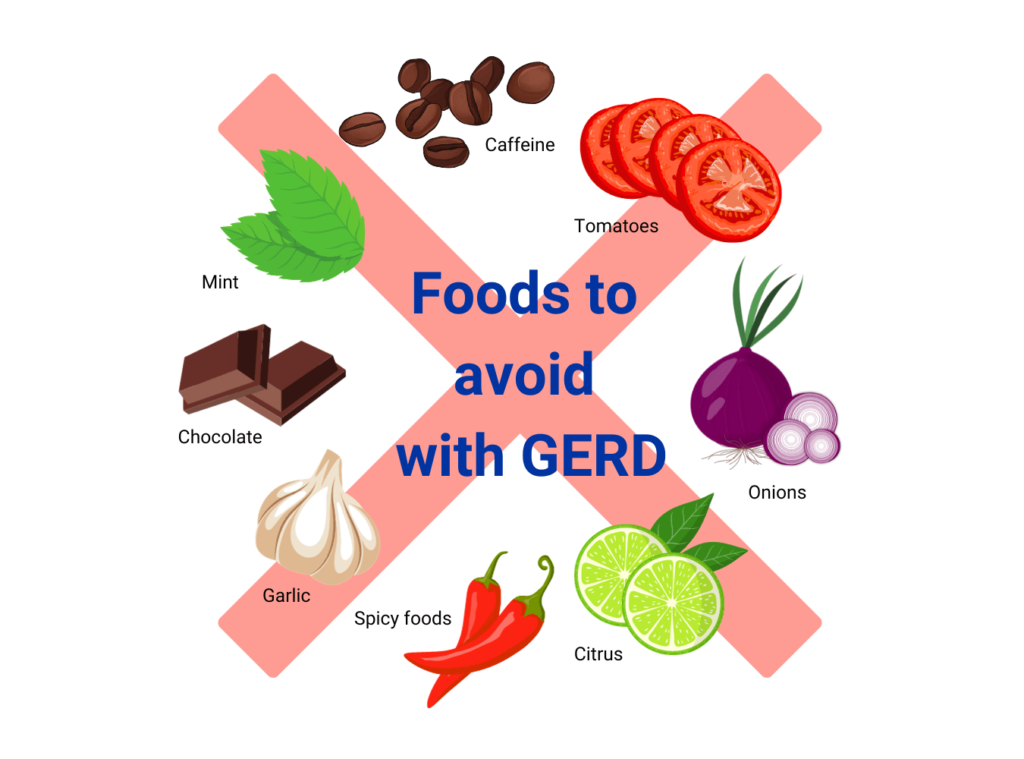
Making changes to your diet can significantly impact GERD management. Avoid triggers like spicy foods, citrus fruits, tomatoes, chocolate, mint, garlic, onions, and caffeinated or carbonated drinks. Since big meals can overstuff your stomach and increase the risk of acid reflux, it’s better to eat smaller meals. Limiting fatty foods is also key, as they can delay stomach emptying and raise the risk of reflux. To prevent nighttime symptoms, hold off on food 2-3 hours before bed.
Managing GERD isn’t only about changing your diet, but also improving your eating habits. Practice good eating posture by keeping your head elevated, and avoid hunching over your plate. Instead, chew your food thoroughly, breathe between bites, and eat slowly to encourage smoother digestion.
Lifestyle Changes
Lifestyle adjustments can also play a crucial role in managing GERD. Elevating the head of your bed can prevent acid from flowing back into the esophagus while sleeping. This can be achieved by using a wedge pillow or placing blocks under your bedpost. Steer clear of tight-fitting clothes because they squeeze your stomach, adding extra pressure. Additional GERD lifestyle changes include losing weight, quitting smoking, cutting back on alcohol, and scheduling regular check-ups to keep an eye on your condition and fine-tune your treatments.
Medications
If you’ve made the GERD lifestyle changes mentioned above but are still experiencing symptoms, think about trying medication. Options include H2 blockers like ranitidine or famotidine, and proton pump inhibitors such as omeprazole or esomeprazole. Over-the-counter antacids like Tums or Rolaids can quickly relieve GERD symptoms like heartburn, but may not be effective for symptoms caused by issues other than acid levels, such as a malfunctioning LES or non-acid reflux.
Surgery
In cases where other treatments are ineffective, surgical options like fundoplication may be considered. This procedure involves wrapping the top part of the stomach around the LES to strengthen it and prevent reflux. Keep in mind that surgery is typically seen as the last step in treating GERD, pursued only after you’ve tried all the less invasive options first.
The Link Between GERD and Stress
GERD and stress are often related because the latter can lead to increased consumption of alcohol, caffeine, fatty foods, and smoking—all of which are behaviors known to aggravate GERD symptoms. Stress is also believed to boost the production of stomach acid, leading to more frequent or severe GERD symptoms. It can slow down stomach emptying, causing food to linger longer in the stomach. This reduces saliva production, which is vital for neutralizing stomach acid and clearing it from the esophagus.
When stress causes the body to be in a ‘fight or flight’ mode, it causes changes in the digestive system, potentially triggering symptoms of GERD. Furthermore, stress can induce muscle tension throughout the body, including in the digestive tract. This tension can affect the digestive system’s functioning and exacerbate GERD symptoms.
Managing stress is undoubtedly crucial for reducing GERD symptoms. Techniques like acupuncture, herbal treatments, meditation, and yoga can provide significant relief. Engaging in regular exercise, getting ample sleep, and practicing efficient time management are also beneficial. Activities like hanging out with friends, going outside, watching your favorite shows, and spending time with children go a long way in restoring your inner peace.
Reaching out to friends and family during stressful times, setting clear work boundaries, taking breaks, and minimizing exposure to stressors can help keep you calm. Seeking a therapist specializing in cognitive-behavioral therapy or stress management, or exploring biofeedback and neurofeedback to manage physiological responses and reduce muscle tension, can also be effective strategies.
Navigate Life Beyond GERD’s Grip
Effective GERD management involves a holistic approach of dietary modifications and lifestyle adjustments. And when needed, medication and surgical interventions can play a part in your GERD recovery process as long as it’s under the consistent guidance of a qualified healthcare professional. Chronic stress plays a significant role in exacerbating GERD, so actively pursuing a less stressful lifestyle is a crucial part of keeping GERD symptoms at bay. Embracing this comprehensive strategy not only helps keep GERD under control but also paves the way for a healthier life, free from the daily discomfort of ongoing tummy troubles.